Diabetic Retinopathy
What is Diabetic Retinopathy?
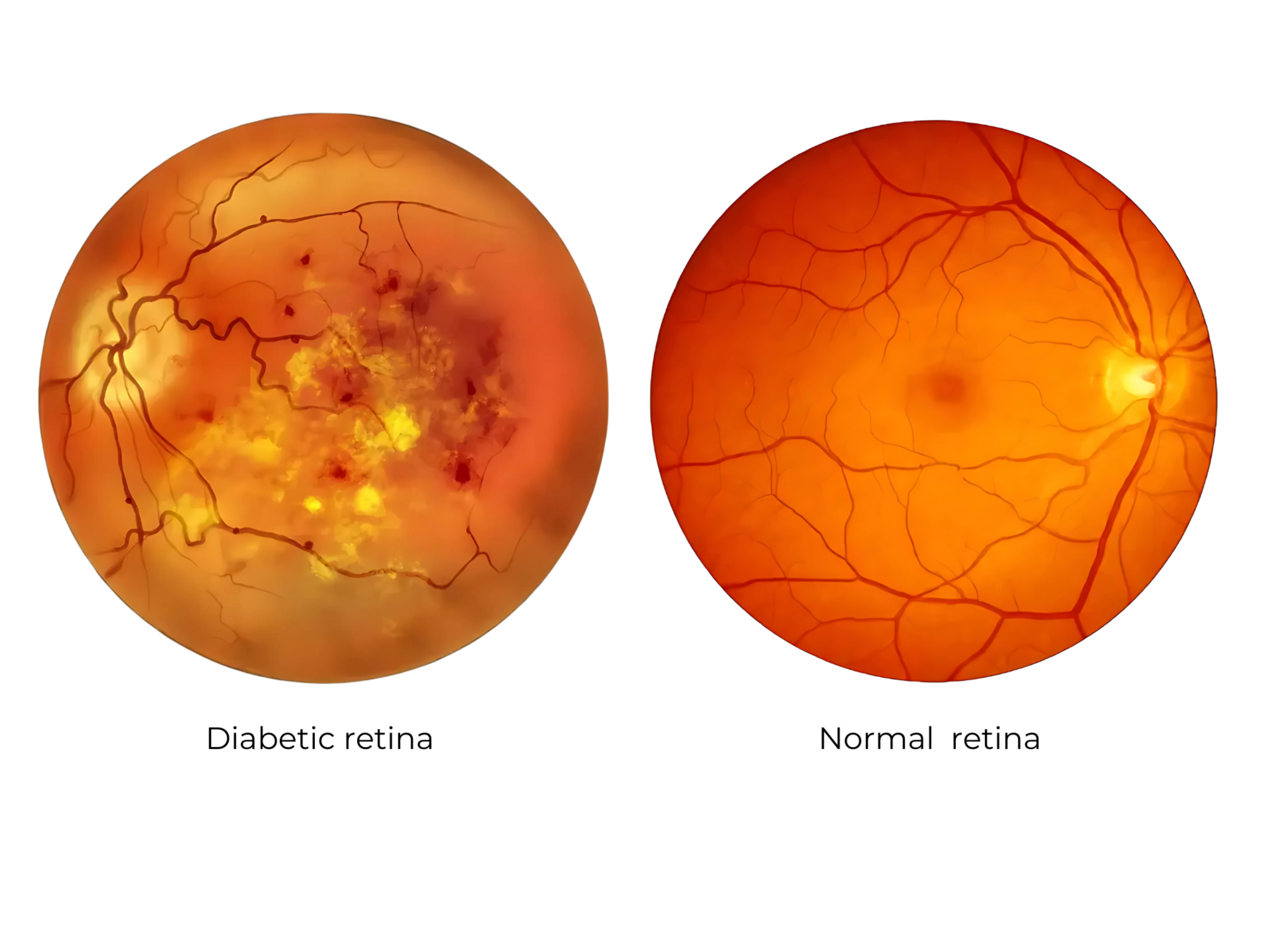
Diabetic retinopathy is a complication of diabetes that damages the blood vessels in the retina, the part of the eye responsible for detecting light and sending signals to the brain. This condition can lead to vision problems and even blindness if not managed effectively.
Stages of Diabetic Retinopathy:
- Non-Proliferative Diabetic Retinopathy (NPDR):
- Early stage; blood vessels in the retina weaken.
- Signs include:
- Microaneurysms: Tiny bulges in blood vessels that may leak fluid.
- Retinal swelling (edema) or hemorrhages (tiny bleeds).
- Hard exudates: Deposits of cholesterol or fats.
- Macular edema: Swelling of the macula, critical for central vision.
- Proliferative Diabetic Retinopathy (PDR):
- Advanced stage; new, abnormal blood vessels grow on the retina.
- Signs include:
- Neovascularization: Fragile, new blood vessels prone to bleeding.
- Vitreous hemorrhage: Bleeding into the gel-like substance inside the eye.
- Retinal detachment: Pulling of the retina due to scar tissue.
- Severe vision loss.
Stages and Effects of Diabetic Retinopathy
1. Early Stage: Non-Proliferative Diabetic Retinopathy (NPDR)
- Blood Vessel Damage: The small blood vessels in the retina weaken, causing them to swell and form microaneurysms.
- Fluid Leaks: Damaged vessels may leak fluid or blood into the retina, leading to swelling (edema).
- Vision Changes: Symptoms may be minimal or nonexistent at this stage, but you might notice blurry vision if macular edema develops (swelling in the central part of the retina).
2. Advanced Stage: Proliferative Diabetic Retinopathy (PDR)
- New Blood Vessel Growth: As damage worsens, the retina signals for the growth of new, abnormal blood vessels (neovascularization).
- Fragility of New Vessels: These new vessels are fragile and prone to leaking blood into the vitreous (the gel-like substance in the eye). This can cause dark spots or floaters in your vision.
- Scar Tissue Formation: Scar tissue from these abnormal vessels can pull on the retina, leading to retinal detachment—a serious condition that can cause permanent vision loss.
Complications of Diabetic Retinopathy
- Macular Edema: Swelling in the macula (the central part of the retina) leads to blurry or distorted vision.
- Vitreous Hemorrhage: Bleeding into the vitreous causes sudden vision changes or complete loss of vision in severe cases.
- Retinal Detachment: Scar tissue pulls the retina away from its underlying layer, causing vision loss if not treated promptly.
- Glaucoma: Increased pressure in the eye can damage the optic nerve, compounding vision problems.
Key Symptoms to Watch For
- Blurry vision
- Dark spots or floaters
- Difficulty seeing at night
- Sudden loss of vision
Why Early Detection Matters
Diabetic retinopathy often has no symptoms in its early stages, making routine comprehensive eye exams critical. Early detection allows for timely treatments, such as laser therapy or anti-VEGF injections, to slow or prevent progression and protect your vision.
Treatment:
1. Early Stages (NPDR):
- Monitoring: Regular eye exams.
- Control of diabetes: Maintain optimal blood sugar, blood pressure, and cholesterol levels.
2. Advanced Stages (PDR or Macular Edema):
- Laser therapy (photocoagulation):
- Reduces abnormal blood vessel growth and leakage.
- Intravitreal injections:
- Anti-VEGF drugs (e.g., ranibizumab, aflibercept, or bevacizumab) to reduce neovascularization and swelling.
- Steroids for macular edema in some cases.
- Vitrectomy:
- Surgery to remove blood or scar tissue from the vitreous gel.
Prevention vision loss from diabetic retinopathy:
1. Manage Blood Sugar Levels
- Keep blood glucose levels within your target range to reduce damage to blood vessels in the retina.
- Monitor blood sugar regularly and adjust your diet, activity, or medication as advised by your healthcare provider.
2. Control Blood Pressure and Cholesterol
- High blood pressure and cholesterol can worsen diabetic retinopathy by increasing stress on blood vessels.
- Take prescribed medications, maintain a heart-healthy diet, and exercise regularly to manage these conditions.
3. Get Regular Eye Exams
- Schedule a comprehensive dilated eye exam at least once a year, even if you don’t have symptoms.
- Early detection can lead to treatments that prevent or minimize vision loss.
4. Adopt a Healthy Lifestyle
- Stay physically active to improve overall blood circulation and metabolic health.
- Avoid smoking, as it can increase the risk of complications from diabetic retinopathy.
5. Follow Through with Treatment
- If diabetic retinopathy is detected, adhere to treatment plans such as laser therapy, anti-VEGF injections, or surgery.
- Consistently follow up with your eye care specialist to monitor and manage the condition effectively.
2.png)
3.png)